Naloxone – Opioid Overdose Treatment
What is Naloxone?
Naloxone is a drug that acts as an antidote to reverse the effects of an opioid overdose, by blocking the action of the opioid at the receptor level.
The most important point of this entire article is this:
Naloxone can save the life of a person who is experiencing an opioid overdose!
An opioid is sometimes called a narcotic, and is typically prescribed as a pain reliever. Opioids are also commonly abused because of the intense feelings of euphoria they also produce. In addition, they are highly addictive, and if sufficient amount is taken an opioid overdose occurs which can cause difficulty in breathing, coma, and death. Statistics are clear that overdose death rates in general and especially the number of deaths from opioid overdose have skyrocketed in recent years. Examples of opioids include:
- Heroin
- Morphine
- Fentanyl
- Oxycodone (Oxycontin)
- Methadone
- Hydrocodone (Vicodin)
- Codeine
- Buprenorphine (Suboxone)
Naloxone has been used for decades by paramedics and in hospitals to reverse the effects of opioid overdose. Naloxone is also used to help diagnose whether an unresponsive person has used an overdose of an opioid. The drug is legal and is approved by the Food and Drug Administration (FDA). This somewhat miraculous substance works by neutralizing the opioids in a person's system. Naloxone only works if a person has opioids in their system, and it does not work on other drugs. A person can not get high on Naloxone and it is thought to be safe for nearly everyone. Naloxone can be administered by injecting into the muscle, into the vein or artery, or in a spray that is inhaled into the nose.
History of Naloxone
Naloxone was patented in 1961 by Jack Fishman, Mozes J. Lewenstein, and Daiichi Sankyo, a large Japanese pharmaceutical company. The active pharmaceutical ingredient Naloxone Hydrochloride received FDA approval for use on opioid overdose in 1971. Injectable Naloxone over the next 40 years became the standard of care used by emergency medical first responders and within the hospital setting for treatment of opioid overdose.
As opioid-related deaths continued to increase, Naloxone was increasingly tested for use outside of the professional medical setting. In 1996, for example, local pilot programs began distributing naloxone to opioid users and laypersons in several major metropolitan areas across the US. These programs achieved positive results, but because this version of the drug was still injectable, it required training to administer, and also posed a risk for infectious disease transmission.
In 2013 the Substance Abuse and Mental Health Services Administration (SAMHSA) introduced the Opioid Overdose Toolkit, a federal resource promoting safety and prevention information for people at risk for overdose. Topics in the toolkit include:
- Naloxone in preventing fatal opioid overdose
- An overview of the safety of Naloxone
- The importance of access to naloxone
In 2014 Evzio, a Naloxone auto-injector, was approved by the FDA. This is an injectable version that was designed to be safe and easy to use for non-professionals. Evzio is approved for immediate administration by friends or family as emergency treatment for overdose in settings such as in the home.
Also in 2014, researchers at the University of Kentucky announced progress on an inhalable form of Naloxone. The product was fast tracked for approval by the FDA, and intranasal Naloxone was approved for use by the FDA in 2015.
The SAMHSA Opioid Overdose Toolkit mentioned above has also been updated, and now recommends that healthcare professionals should consider prescribing Naloxone along with a patients’ initial opioid prescription.
Naloxone is one of the drugs on the World Health Organization's List of Essential Medicines, which was constructed to include the most important medications needed in any basic health care system. Naloxone is available as a generic medication and is an inexpensive drug.
Naloxone is available without a prescription in many states, but some states still require a prescription. There is a strong movement to make Naloxone easily available everywhere, so that more lives are saved.
Physiology of Naloxone
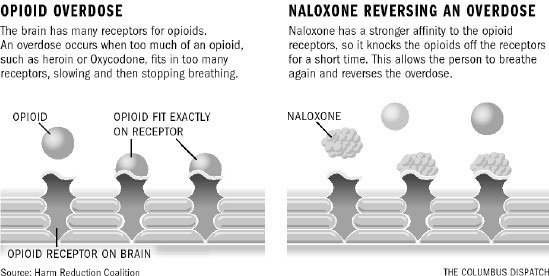
Opioids bind to many different receptors on the brain. When an overdose occurs too many opioid molecules are present and they block all the receptors. This slows breathing, eventually causing it to stop.
Naloxone works because it has a stronger ability to bind to the opioid receptors in the human brain than the opiods themselves. Thus the Nalaxone molecules essentially "push" the opioid molecules off the receptors temporarily, thereby blocking their effects.
Signs of an Opioid Overdose
A person who has overdosed may:
- be breathing very slow or not breathing at all
- have a slow heartbeat
- have blue or purplish lips or fingernails
- have very small or pinpoint pupils in the eyes
- be limp
- be vomiting or gurgling
- not wake up or respond to stimulus
If you think a person shows signs of an overdose you should:
- Call 911 immediately.
- Begin rescue breathing, if the person is not breathing.
- Administer Naloxone to the person.
Administration of Naloxone
Naloxone is given by injection shot or by nasal spray. Follow all medication instructions carefully.
The injectable version of Naloxone is called Evzio, and is injected into a muscle in the outer thigh area. In an emergency, you may give an injection through the person's clothing. After injecting Naloxone, make sure to stay with the person and watch for continued signs of overdose. You may need to give additional injections every 2 to 3 minutes until emergency help arrives. Each Evzio Naloxone auto-injector is for one use only. Throw away after one use, even if there is still some medicine left in it after injecting a dose.
The inhalant version of Naloxone is called Narcan, and is sprayed into the person's nose. As with the injectable version, if there is no response and more doses are available, administer additional doses of every 2 to 3 minutes using a new device with each dose until emergency medical assistance arrives.
It is extremely important to not assume that an overdose episode has ended, and that the person is out of danger if symptoms improve. You must get emergency help after administering Naloxone.
Opioid Addiction Treatment
Opioids are highly addictive, and it is extremely difficult and dangerous to attempt to stop their use on one's own accord. A person who is addicted to opioids becomes both physically and psychologically dependent. But even though severe consequences may occur because of the addiction, they are often afraid to stop using for fear of the withdrawal symptoms they may experience caused by that same dependence. Thereby a vicious cycle of stopping use and starting again often perpetuates itself indefinitely in the addicts life.
One of the biggest challenges in getting an addict to seek treatment for opioid addiction is to overcome the fear they associate with the withdrawal process. Making this process as comfortable as possible can be the deciding factor in bringing an opioid addict into treatment. Only after stopping use does the person have a chance for lasting recovery.
The Anaheim Lighthouse Opioid Addiction Treatment Program features a medically supervised drug detox program. Once stabilized through the detox process the individual can then enter one of our residential treatment or intensive outpatient treatment programs. This choice depends on the individual and their situation. An Anaheim Lighthouse admissions adviser can help you or your loved one decide on the proper treatment program and the appropriate length of stay in treatment. We use a variety of therapeutic methods in a highly contemporary approach to treatment for Opioid Addiction.
Anaheim Lighthouse is located on a residential campus in beautiful and sunny Anaheim in Southern California. Please contact one of our professional and compassionate team at 877-959-5909 today to discuss Opioid Addiction Treatment options for you or your loved one.